Board Prep: Overview of Donor Infectious Disease Eligibility
- Dec 28, 2025
- 5 min read
Donor infectious disease eligibility is one of those topics that feels straightforward until you’re asked to explain why a donor with negative testing still isn’t eligible — or why some pathogens get NAT, others don’t, and some only get tested once.
This post walks through donor eligibility the way the boards expect you to understand it: as a risk-assessment framework, not just a checklist of tests.
What Is Donor Infectious Disease Eligibility?
Donor eligibility is the assessment of a donor’s risk of transmitting infectious disease to a recipient. Its purpose is recipient protection and it is based on two pillars:
Donor history
Laboratory testing
This is distinct from donor suitability, which focuses on donor safety (for example, hemoglobin thresholds or procedural tolerance). A donor can be suitable but not eligible — and vice versa.
How Donor Eligibility Is Determined
The Donor History Questionnaire (DHQ)
The DHQ evaluates risks that laboratory testing alone cannot fully capture, including:
Symptoms of infection
Behavioral risk factors
Travel and residence history
Exposure history (blood, needles, sexual contact)
Testing does not eliminate window-period risk, and emerging pathogens may not yet have validated screening assays. As a result, negative testing does not equal eligibility when exposure risk is recent.
The Window Period (Why History Still Matters)
The window period is the time between infection and when that infection becomes detectable by testing.
Even with modern NAT-based screening, window periods still exist. This is why donor history remains a critical component of eligibility determination.
Infectious Disease Screening: The Tests (What We Use and Why)
All allogeneic donors undergo infectious disease screening using serologic testing, nucleic acid testing (NAT), or both. The strategy used for each pathogen reflects its biology: duration of viremia, durability of antibody response, prevalence, and the clinical consequences of transmission.
HIV-1/2
Serology
HIV-1/2 antibody
HIV-1 p24 antigen
NAT
HIV-1 RNA
Window Period
NAT: 9–11 days
Serology: 15–20 days
Notes
Layered NAT and Ag/Ab screening minimizes window-period transmission, making residual transfusion-transmitted HIV risk extremely low. However, there is no licensed HIV-2 NAT test in the U.S., so HIV-2 detection relies entirely on serology.
Hepatitis B Virus (HBV)
Serology
HBsAg
Anti-HBc
NAT
HBV DNA
Window Period
NAT: 20–22 days
Serology: 30–38 days
Notes
HBV has the longest residual transfusion risk among routinely screened viral infections due to low-level, intermittent viremia. Triple-layer testing mitigates occult and low-level infection but does not eliminate risk entirely.
Hepatitis C Virus (HCV)
Serology
Anti-HCV
NAT
HCV RNA
Window Period
NAT: 3–5 days
Serology: 50–70 days
Notes
Universal NAT has nearly eliminated window-period HCV transmission. Anti-HCV testing is notorious for false positives, which is why donor re-entry policies matter.
HTLV-I/II
Serology
Anti-HTLV-1/2
NAT
Not performed
Window Period
Serology: 45–60 days
Notes
HTLV infection is chronic with a durable antibody response, enabling serology-only screening. HTLV-1 is associated with adult T-cell leukemia/lymphoma. The screening strategy reflects low prevalence, not a short window period.
West Nile Virus (WNV)
Serology
Not performed
NAT
WNV RNA
Window Period
NAT: 6–10 days
Notes
Short viremia necessitates NAT-only, seasonally adaptive screening. Serology is not useful for donor screening in acute infection.
Syphilis (Treponema pallidum)
Serology
Treponemal antibody test
Non-treponemal test
NAT
Not performed
Window Period
Serology: 10–30 days
Notes
T. pallidum survives poorly in refrigerated blood, making transfusion transmission rare but documented. Treponemal antibodies persist long after infection and treatment, which is why syphilis is a key context for donor re-entry.
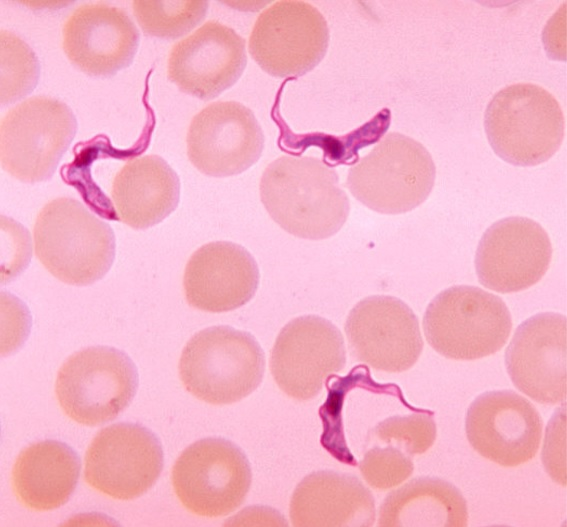
Trypanosoma cruzi (Chagas Disease)
Serology
Antibody testing only
NAT
Not performed
Window Period
Serology: 3–8 weeks
Notes
Chronic infection with durable antibodies enables one-time serologic screening. Transmission is rare but serious and linked to donors with residence in endemic areas.
Babesia
Serology
Not performed
NAT
Babesia DNA
Window Period
NAT: 7–14 days
Notes
Persistent asymptomatic parasitemia necessitates regional NAT screening. Babesia is a leading cause of fatal transfusion-transmitted infection in the U.S., with required testing in endemic regions including the Northeast and Upper Midwest.
Deferrals: Temporary vs Indefinite
Temporary deferrals apply when risk decreases with time
Indefinite deferrals apply when risk does not meaningfully decrease
Examples include:
Temporary: recent tattoo, recent exposure, acute illness
Indefinite: HIV, chronic HBV, HCV, HTLV, vCJD risk
High-Yield Deferral Periods (Boards Love These)
Some deferrals are particularly high yield because they test whether you understand current, risk-based policy rather than outdated rules.
Malaria
Travel to endemic area (no illness): 3-month deferral
Residence in endemic area or prior malaria: 2-year deferral
High-Risk Sexual Behavior or Injection Drug Use
Universal 3-month deferral
Applies regardless of gender or sexual orientation
Incarceration
>72 hours: 12-month deferral
<72 hours: No deferral
Tattoos
State-licensed facility: No deferral
Non-state-licensed facility: 3-month deferral
vCJD-Related Risks
Residence in Great Britain or Europe: No deferral
Use of bovine growth hormone: Indefinite deferral
Cadaveric dura mater transplant: Indefinite deferral
Donor Eligibility Potpourri (The Real-World Stuff)
Donor Re-Entry
Donor re-entry allows individuals with false-positive screening tests to become eligible to donate again. This process:
Is pathogen-specific
Is regulated by the FDA
Requires repeat testing on a subsequent donation
Confirmed infections generally preclude re-entry, with syphilis (after full treatment) being the main exception.
Product Look-Backs
Product look-backs occur when a donor is later found to have a positive infectious disease test. All donations during a defined prior period must be investigated to determine:
Whether products were transfused
Whether recipient notification or testing is required
For boards:
Look-backs are mandated for HIV-1/2 and HCV
The required look-back period is 12 months prior to the positive test
Special Donor Populations
Directed Donors
Must meet the same infectious disease eligibility criteria
No relaxation of standards
If unused, products may be returned to general inventory
Autologous Donors
Minimum hemoglobin: >11 g/dL
Collection must occur >72 hours before surgery
Requires physician order
Infectious disease testing may vary by institutional policy
If unused, products are discarded
Regulatory Oversight: Who Sets the Rules?
FDA
Establishes laws and regulations
21 CFR 630 governs donor infectious disease testing
AABB
Interprets FDA regulations into operational standards
Maintains the Donor History Questionnaire
Understanding who regulates what matters — especially when policies change.
Consolidated Board Pearls
The Basics
Define the window period → Time between infection and detection
What does DHQ stand for? → Donor History Questionnaire
Infectious Disease Screening
Name 3 pathogen classes not directly tested → Most bacteria, most parasites, prion diseases
Screening Tests
Most common fatal transfusion-associated infection? → Babesia
HIV-1/2 NAT window period? → 9–11 days
Virus with longest residual transfusion risk? → HBV
Deferrals
Universal deferral period for high-risk behavior? → 3 months
Deferral for incarceration <72 hours? → None
Deferral for cadaveric dura mater transplant? → Indefinite
Eligibility Potpourri
Mandated look-back period for HIV? → 12 months
What is donor re-entry? → Process allowing donors with false-positive tests to donate again
If a directed unit is unused, must it be discarded? → No, it may enter general inventory



